It often starts with a missed period, sudden acne flare-ups, or stubborn weight gain that just won't go away despite your best efforts. If you are an Indian woman in 2026—whether navigating the fast-paced life of Mumbai or managing a household in rural Punjab—you are likely hearing two terms repeatedly: PCOD and PCOS.
In the last decade, hormonal health issues in India have escalated from a medical concern to a silent epidemic. But amidst the noise of social media advice and outdated myths, the fundamental question remains: What exactly is happening to my body?
- 1. Introduction: The Silent Epidemic in India
- 2. PCOD vs. PCOS: Deep Dive Comparison (The Core Difference)
- 3. Signs and Symptoms: Decoding Your Body’s Signals
- 4. Causes and Risk Factors: Why is this happening to me?
- 5. Diagnosis and Tests: Beyond the Ultrasound
- 6. Comprehensive Treatment Protocols (Medical & Holistic)
- 7. The Ultimate Indian Diet for PCOD/PCOS (The Game Changer)
- 8. Exercise and Lifestyle Management
- 9. Pregnancy, Fertility and Life Stages
- 10. Long-term Complications and Prevention
- 11. Myths vs. Facts: Busting Common Misconceptions
- 12. Conclusion: Taking Charge of Your Health in 2026
1. Introduction: The Silent Epidemic in India
According to the latest 2026 health surveys, nearly 1 in 5 Indian women suffer from hormonal imbalances. The confusion, however, begins with the names themselves. Many women use these terms interchangeably, but medically, they define two distinct trajectories of health.
Quick Definitions (The Basics)
- What is PCOD? The full form of PCOD is Polycystic Ovarian Disease. It is largely a lifestyle-induced condition where ovaries produce immature eggs.
- What is PCOS? The full form of PCOS is Polycystic Ovary Syndrome. This is a more severe metabolic disorder involving the endocrine system and high male hormones.
1.1 The 2026 Perspective: Why Now?
Why did our grandmothers rarely discuss PCOD or its symptoms? The answer lies in the drastic shift in the Indian lifestyle over the last 20 years. In 2026, we are battling factors that didn't exist previously:
- Endocrine Disruptors: Microplastics in our water and food packaging are mimicking hormones, confusing our reproductive systems.
- The "Sitting" Pandemic: Whether it's IT jobs in Bengaluru or mechanized farming in villages, physical movement has hit an all-time low.
- Stress & Cortisol: The pressure to balance modern careers with traditional expectations is spiking cortisol levels in Indian women, which directly disrupts ovulation.
Understanding whether you have PCOD or PCOS is the first crucial step toward taking control. Let’s decode the differences.
2. PCOD vs. PCOS: Deep Dive Comparison (The Core Difference)
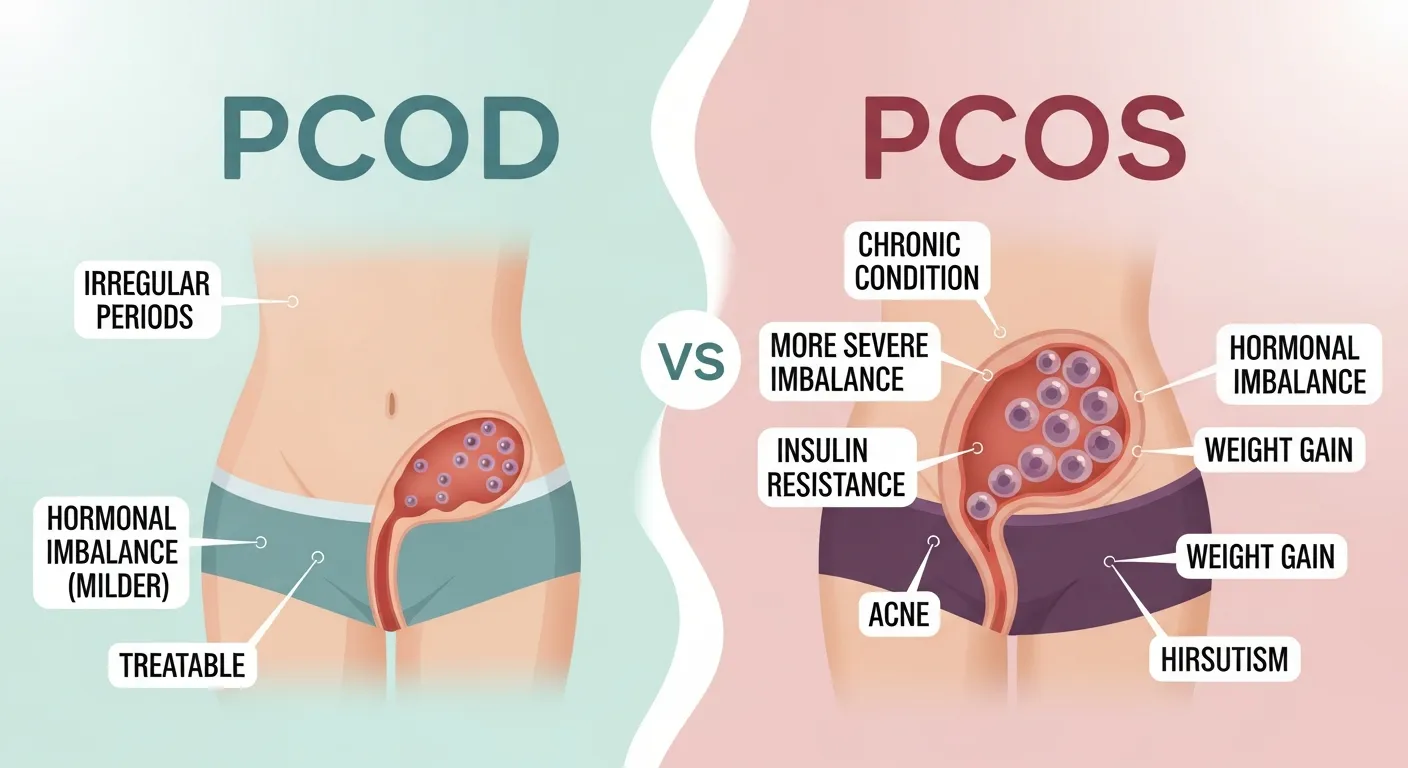
When you get your ultrasound report, seeing the word "Polycystic" can be scary. However, the difference between having the "Disease" and the "Syndrome" is massive. To get the best treatment, you must understand the mechanism behind PCOS and PCOD.
2.1 What is PCOD (Polycystic Ovarian Disease)?
Think of PCOD as a "factory jam." In a healthy cycle, your ovaries release one mature egg every month. In Polycystic Ovarian Disease (PCOD), the ovaries produce many immature or partially mature eggs. Instead of being released, these eggs turn into small cysts (fluid-filled sacs).
Key Characteristic: The ovaries become enlarged, but they often continue to function partially. PCOD is heavily influenced by diet and lifestyle. For many Indian women, simply correcting their protein intake and sleep cycle can reverse PCOD completely.
2.2 What is PCOS (Polycystic Ovary Syndrome)?
PCOS is far more complex. It is not just about the ovaries; it is a Metabolic Disorder. The full form of PCOS points to a "Syndrome"—which means a group of symptoms affecting the whole body.
In PCOS, the body struggles with Insulin Resistance. High insulin levels trigger the ovaries to produce excessive Androgens (Male Hormones like Testosterone). This hormonal chaos stops ovulation entirely, leads to male-pattern hair growth, and increases the risk of heart disease and diabetes.
2.3 PCOD vs PCOS: The Ultimate Comparison Table
Use this detailed chart to understand where you stand. This is the most updated comparison based on 2026 medical standards.
| Feature | PCOD (Polycystic Ovarian Disease) | PCOS (Polycystic Ovary Syndrome) |
|---|---|---|
| Full Form | The pcod full form is Polycystic Ovarian Disease. | The pcos full form is Polycystic Ovary Syndrome. |
| Nature of Condition | A temporary condition caused largely by lifestyle imbalances. | A chronic metabolic disorder affecting the endocrine system. |
| Prevalence in India | Very Common (Approx. 25% of women). | Less Common but more severe (Approx. 10% of women). |
| Ovarian Function | Ovaries contain immature eggs but may still ovulate irregularly. | Ovaries stop releasing eggs (Anovulation) due to high male hormones. |
| Fertility & Pregnancy | Women can usually conceive naturally with minor lifestyle tweaks. | Conception is difficult; requires medical intervention and ovulation induction. |
| Primary Symptoms | Irregular periods, abdominal weight gain. | Facial hair (Hirsutism), severe acne, hair loss, skin darkening. |
| Long-term Risks | Minimal risk if managed. | High risk of Type 2 Diabetes, Hypertension, and Endometrial Cancer. |
2.4 Why the Distinction Matters for Treatment
If you have PCOD, your doctor might focus purely on Diet and Exercise (cutting sugar and increasing movement). However, if you have PCOS, the treatment will be multi-dimensional, involving:
- Endocrinologists: To manage insulin resistance.
- Dermatologists: To treat hormonal acne and hair growth.
- Gynaecologists: To regulate cycles and protect the uterus.
In the next section, we will decode the signs and symptoms—specifically focusing on how they appear on Indian skin and body types—so you can spot the red flags early.
3. Signs and Symptoms: Decoding Your Body’s Signals
PCOS is often called "The Thief of Womanhood" because it slowly steals physical traits associated with femininity—hair, skin texture, and body shape—and replaces them with male-pattern symptoms. In 2026, doctors look beyond just your menstrual dates. They look at the "Indian Phenotype" of PCOS.
If you are wondering, "Do I have PCOS or is it just stress?", cross-check your body against these symptoms.
3.1 The Visible Physical Symptoms
- Central Obesity (The "PCOS Belly"): Unlike general weight gain, Indian women with PCOS tend to accumulate fat specifically around the lower abdomen (tummy area). You might have thin arms and legs but a protruding belly. This is a direct sign of Insulin Resistance.
- Hirsutism (Unwanted Hair Growth): Are you finding yourself visiting the parlour for threading more often? Thick, coarse, dark hair appearing on the chin, upper lip, jawline, chest, or belly button is caused by high Androgen (testosterone) levels.
- Adult Acne: This isn't teenage pimples. PCOS acne typically appears along the "U-Zone" (jawline and chin), is cystic (painful bumps under the skin), and flares up right before a period is due.
- Male-Pattern Baldness (Androgenic Alopecia): While hair grows on the face, it falls from the scalp. You may notice your hair partition (maang) becoming wider or thinning specifically at the front and crown of the head.
3.2 Skin Signs: The "Dark Patch" Warning
Do you have dark, velvety patches on the back of your neck, underarms, or groin area? Many women scrub this thinking it is dirt or tan. It is not dirt. It is a skin condition called Acanthosis Nigricans, caused by high insulin levels in the blood. It is often the very first sign of PCOS in young Indian girls.
3.3 Menstrual and Internal Symptoms
- Oligomenorrhea: Having fewer than 9 periods in a year. Cycles may be delayed by 35 days to 6 months.
- Heavy Menstrual Bleeding: When periods finally arrive after a long gap, the uterine lining (which has been building up) sheds all at once. This leads to heavy flow, clots, and severe pain.
- Pelvic Pain: A dull ache in the lower abdomen or back, often unrelated to periods, caused by enlarged ovaries pressing on pelvic organs.
3.4 The Hidden Mental Health Toll
PCOS is not just physical; it is psychological. Fluctuating hormones affect neurotransmitters in the brain.
- Anxiety & Depression: Studies in India show that women with PCOS are 3 times more likely to suffer from anxiety, often triggered by body image issues (weight/hair) and fertility fears.
- Fatigue & Sleep Apnea: Do you wake up tired even after 8 hours of sleep? Insulin resistance causes energy crashes, and weight gain can lead to obstructive sleep apnea (snoring/breathing pauses).
4. Causes and Risk Factors: Why is this happening to me?
One of the most common questions doctors hear is: "Why me? I eat home-cooked food, so why do I have this?"
The development of Polycystic Ovarian Disease (PCOD) or PCOS is rarely due to a single cause. It is a "Perfect Storm" of genetics, environment, and lifestyle colliding together.
4.1 Insulin Resistance: The Root Cause
For almost 70% of Indian women with PCOS, the root cause is Insulin Resistance. Here is how it works:
- The Lock & Key Failure: Insulin is a hormone that acts like a key to open your body's cells so they can absorb sugar (glucose) for energy.
- The Resistance: In PCOS, your cells change the locks. The "key" (insulin) doesn't work effectively.
- The Overload: Your body notices blood sugar is still high, so the pancreas pumps out more insulin to force the cells open.
- The Ovarian Error: High levels of insulin travel to the ovaries. Unfortunately, ovaries are very sensitive to insulin. This excess insulin triggers the ovaries to produce Testosterone instead of Estrogen.
- Result: Ovulation stops, and male symptoms (hair growth) begin.
4.2 Genetics: The "Thrifty Gene" Hypothesis
If your mother, aunt, or sister has PCOS, diabetes, or irregular periods, your risk increases by 50%. South Asians have historically evolved to survive famines, meaning our bodies are genetically programmed to store fat easily (The Thrifty Gene).
4.3 The Urban vs. Rural Lifestyle Shift (2026 Context)
| Factor | Urban India Impact | Rural India Impact |
|---|---|---|
| Diet | High intake of processed carbs (Maida, Pizza, Burgers) and hidden sugars in "health drinks." | High carb intake (Rice/Roti) with very low protein. Increased pesticide use in local farming acting as toxins. |
| Activity | Sedentary desk jobs, long commutes, dependence on elevators and delivery apps. | Mechanization of farming and household chores has drastically reduced daily physical labor. |
| Sleep | "Revenge Bedtime Procrastination"—staying up late scrolling phones disrupts the circadian rhythm. | Better sleep cycles generally, but rising stress levels regarding finances and family. |
4.4 Endocrine Disruptors (The Modern Enemy)
In 2026, we are exposed to chemicals that confuse our hormones, known as Endocrine Disrupting Chemicals (EDCs). Common sources include:
- Plastics: Drinking hot tea/coffee in plastic cups or eating hot food from plastic containers releases BPA/Phthalates.
- Adulterated Milk: Presence of oxytocin or growth hormones in dairy cattle can affect human hormones.
- Cosmetics: Parabens and sulfates found in everyday shampoos and lotions can mimic estrogen in the body.
4.5 Chronic Low-Grade Inflammation
Women with PCOS often have low-level inflammation (similar to what happens when you have a mild infection, but permanent). This prompts polycystic ovaries to produce androgens, which can lead to heart and blood vessel problems later in life.
5. Diagnosis and Tests: Beyond the Ultrasound
In India, a common misconception is that if your Ultrasound report says "Polycystic Ovaries," you definitely have the disease. This is not true. Almost 20% of healthy women can have cystic ovaries without having the syndrome.
To confirm the diagnosis of PCOS (Polycystic Ovary Syndrome), doctors in 2026 follow the Rotterdam Criteria. You must meet at least two out of the following three conditions:
- Ovulatory Dysfunction: Irregular or missed periods (indicating you aren't releasing eggs).
- Hyperandrogenism: High male hormones found in blood tests OR visible signs like facial hair/acne.
- Polycystic Ovaries: Ultrasound showing enlarged ovaries with multiple small follicles (cysts).
5.1 Essential Blood Tests List
When you visit a gynaecologist or endocrinologist, do not settle for just a scan. Ask for a comprehensive "PCOD Profile." Here is what it must include:
| Test Name | Why it is Important? |
|---|---|
| FSH & LH Ratio | Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH). In a healthy woman, the ratio is 1:1. In PCOS, LH levels are often 2-3 times higher than FSH, which prevents ovulation. |
| Total & Free Testosterone | To check the level of male hormones causing hair growth and acne. |
| Fasting Insulin & HOMA-IR | Most Critical for Indians. It checks for Insulin Resistance. You might have normal blood sugar (Glucose) but very high Insulin, which is the root cause of PCOD. |
| TSH, T3, T4 (Thyroid Profile) | Thyroid issues and PCOD often go hand-in-hand. Hypothyroidism mimics PCOD symptoms like weight gain. |
| AMH (Anti-Müllerian Hormone) | Women with PCOS often have very high AMH levels because they have many immature eggs stored up. |
| Lipid Profile | To check Cholesterol and Triglycerides, as PCOS increases heart disease risk. |
5.2 The Ultrasound (USG) Explained
The doctor will look for the "String of Pearls" sign. This appears when many small immature follicles (cysts) are arranged around the edge of the ovary, looking like a pearl necklace.
Note: For married women, a Transvaginal Scan (TVS) gives a clearer picture than an abdominal scan.
6. Comprehensive Treatment Protocols (Medical & Holistic)
Once diagnosed with PCOD (Polycystic Ovarian Disease) or PCOS, the immediate question is: "Is there a medicine to cure it?"
In 2026, the treatment is not a single pill. It is a "Multi-Modality Approach" combining modern medicine, supplements, and traditional wisdom.
6.1 Standard Medical Management (Allopathic Options)
Depending on whether your primary concern is irregular periods, skin issues, or fertility, a doctor may suggest the following treatment lines:
-
Hormonal Birth Control (Oral Contraceptives):
Often the first step to regulate the menstrual cycle. These pills contain hormones to induce a predictable withdrawal bleed.- How it helps: Lowers androgen levels, reduces acne, and protects the endometrial lining.
- Limitations: They manage symptoms but do not cure insulin resistance. Periods may become irregular again if stopped.
-
Insulin Sensitizers (Metformin):
While primarily a diabetes medication, Metformin is widely used in PCOS management to address the root cause—Insulin Resistance.- How it helps: Improves the body's response to insulin, which may assist in weight management and restarting spontaneous ovulation.
-
Anti-Androgens (e.g., Spironolactone):
If cosmetic symptoms are severe, these medications may be prescribed to block the effect of male hormones on the skin and hair follicles.- How it helps: Effective in managing hirsutism (facial hair) and androgenic alopecia (scalp thinning).
- Note: Often not prescribed if you are trying to conceive immediately due to safety concerns.
-
Ovulation Induction Agents (Letrozole/Clomiphene):
For women planning a pregnancy, these medications are used under medical supervision to stimulate the ovaries.- How it helps: They assist the development and release of a healthy egg, improving chances of conception.
6.2 The 2026 Game Changer: Inositol Supplements
If you research PCOS treatment protocols in 2026, you will find Myo-Inositol at the top. It is a vitamin-like substance (Vitamin B8) that mimics insulin signals.
6.3 Ayurvedic and "Desi" Approach
Since PCOD is prevalent in India, our traditional systems (Ayurveda) offer powerful supportive treatments focusing on Kapha (weight) and Vata (movement) balance.
- Ashwagandha: An adaptogen that lowers Cortisol (stress hormone). High stress = High blood sugar = Worse PCOS. Ashwagandha breaks this cycle.
- Shatavari: Known as the "female tonic," it nourishes the reproductive system and helps balance hormones.
- Kanchanar Guggulu: Often prescribed by Ayurvedic doctors to reduce the size of cysts and correct thyroid function.
- Triphala: Essential for gut health. Many women with PCOS suffer from constipation and bloating; Triphala aids detoxification.
6.4 Surgical Treatment (The Last Resort)
Surgery is rare today. Laparoscopic Ovarian Drilling (LOD) is a procedure where a laser punctures the ovary to destroy testosterone-producing tissue. It is usually only considered if weight loss and medication fail to restart ovulation.
7. The Ultimate Indian Diet for PCOD/PCOS (The Game Changer)
You cannot out-train a bad diet. For Indian women, the biggest challenge is our carbohydrate-heavy culture. Whether it is Parathas in the North or Idli-Dosa in the South, our traditional meals often lack protein and spike insulin levels immediately.
In 2026, the dietary approach for PCOD is not about "starving." It is about Glucose Management. The goal is to keep your blood sugar stable so your insulin doesn't spike and trigger your ovaries to make testosterone.
7.1 Understanding the Glycemic Index (GI)
The Glycemic Index measures how quickly a food raises your blood sugar.
The Rule: Stop eating High GI foods. Start eating Low GI foods.
| Food Category | ❌ AVOID (High GI) - Spikes Insulin | ✅ EAT (Low/Medium GI) - Stable Hormones |
|---|---|---|
| Grains | Maida (Biscuits, Bread, Naan), White Rice, Instant Oats, Suji (Semolina). | Millets (Shree Anna): Jowar, Bajra, Ragi. Brown Rice, Red Rice, Quinoa, Steel-cut Oats. |
| Vegetables | Potatoes (Aloo), Sweet Corn, Yam. | Spinach (Palak), Bhindi, Lauki, Methi, Broccoli, Cauliflower. |
| Fruits | Mango, Chikoo, Grapes, Lychee (High Sugar). | Papaya, Guava, Apple, Pomegranate, Berries, Orange. |
| Fats & Oils | Refined Oils (Soybean, Sunflower), Dalda. | Ghee (in moderation), Coconut Oil, Mustard Oil, Olive Oil. |
| Beverages | Chai with Sugar, Soft Drinks, Packed Juices. | Spearmint Tea, Green Tea, Jeera Water, Black Coffee. |
7.2 The "Plate Method" for Indian Meals
You don't need to calculate calories. Just change your plate ratio:
- 1/2 Plate: Vegetables (Sabzi/Salad) - Fiber slows down sugar absorption.
- 1/4 Plate: Protein (Dal/Chicken/Fish/Paneer/Egg) - Essential for hormone repair.
- 1/4 Plate: Carbohydrates (Roti/Rice) - Keep this portion smallest.
7.3 Regional Diet Options (Urban & Rural)
North Indian PCOD Plan
- Breakfast: 2 Besan Chillas with Paneer filling OR 2 Eggs Omelette with veggies.
- Lunch: 1 Jowar/Bajra Roti + Bowl of Thick Dal + Salad + Curd. (Stop eating 3-4 wheat rotis).
- Dinner: Grilled Chicken/Paneer Tikka or Sautéed Vegetables with Soup.
- Snack: Roasted Makhana or a handful of Walnuts/Almonds.
South Indian PCOD Plan
- Breakfast: Pesarattu (Moong Dal Dosa) with ginger chutney OR Ragi Idli (Limit: 2).
- Lunch: Red/Brown Rice (1 cup) + Sambar (with lots of drumsticks/veggies) + Cabbage Poriyal.
- Dinner: Steamed Fish or Tofu stir-fry. Avoid Rice at night if possible.
- Snack: Sundal (Chickpea salad) or Buttermilk (Chaas).
7.4 Seed Cycling: The Ancient Hormone Hack
Seed cycling involves eating specific seeds during specific phases of your menstrual cycle to support Estrogen and Progesterone.
- Phase 1 (Day 1 to 14 - From period start to ovulation): Eat 1 tbsp Flax Seeds + Pumpkin Seeds. (Boosts Estrogen).
- Phase 2 (Day 15 to 28 - From ovulation to next period): Eat 1 tbsp Sesame Seeds + Sunflower Seeds. (Boosts Progesterone).
8. Exercise and Lifestyle Management
You might be thinking, "I walk 30 minutes daily, why am I not losing weight?"
For patients with PCOS, simple cardio (walking) is often not enough to break severe insulin resistance. You need to build muscle.
8.1 Why Strength Training is Non-Negotiable
Muscles are the biggest consumers of glucose in the body. When you lift weights or do bodyweight exercises (pushups/squats), your muscles become "hungry" for sugar, pulling it out of your blood and lowering your insulin levels naturally.
The Strategy:
Aim for Resistance Training 3-4 days a week.
Examples: Squats, Lunges, Planks, Dumbbell presses. You don't need a gym; water bottles or resistance bands work at home.
8.2 Yoga Asanas for Ovarian Health
Yoga does something gymming cannot—it lowers Cortisol (Stress). High stress directly blocks ovulation. These 3 asanas are clinically recommended for PCOD:
- Badhakonasana (Butterfly Pose): Opens up the pelvic region and increases blood flow to the ovaries.
How to do: Sit with legs straight, bend knees, bring feet together, and flap knees like a butterfly. - Bhujangasana (Cobra Pose): Exerts gentle pressure on the abdomen and massages the reproductive organs.
- Surya Namaskar (Sun Salutation): The ultimate metabolic booster. Doing 10-12 rounds daily can significantly help in weight loss.
8.3 The Sleep-Hormone Connection
In 2026, "Sleep" is considered a medical prescription.
The Science: Hormones are regulated by your Circadian Rhythm. Melatonin (sleep hormone) signals the body to repair itself.
- The 10 PM Rule: Try to sleep by 10 PM. The body's physical repair happens between 10 PM and 2 AM.
- Blue Light: Using phones late at night suppresses melatonin, which in turn disturbs insulin. Avoid screens 1 hour before bed.
8.4 Managing Stress (The Silent Killer)
For the modern Indian woman balancing work and home, stress is constant. Chronic stress keeps Cortisol high. When Cortisol is high, Progesterone (the period-regulating hormone) drops.
Actionable Tip: Practice Pranayama (Anulom Vilom) for 10 minutes daily. It is proven to lower cortisol levels immediately.
9. Pregnancy, Fertility and Life Stages
For an Indian woman, the diagnosis of PCOD often comes with a heavy dose of societal pressure: "Will I be able to become a mother?"
Let us clear the air immediately: Having PCOD or PCOS does NOT mean you are infertile. It means you are "sub-fertile," which simply implies you might need a little more planning and medical help than others.
9.1 Can I get pregnant with PCOD Problem?
Yes. In fact, women with PCOD (Polycystic Ovarian Disease) often conceive naturally just by losing 5-10% of their body weight. Since PCOD is milder, the ovaries still function reasonably well once lifestyle factors are corrected.
For women with PCOS (Polycystic Ovary Syndrome), the challenge is Anovulation (lack of egg release). If there is no egg, sperm cannot fertilize anything. However, with modern medicine in 2026, success rates are very high.
9.2 The "Fertility Ladder" Treatment
If you are trying to conceive, doctors usually follow this step-by-step approach:
- Step 1: Lifestyle Correction (3-6 Months): Diet and Exercise are the first "medicine." Many women ovulate spontaneously after losing belly fat.
- Step 2: Ovulation Induction (Medication): Doctors prescribe oral medicines like Letrozole or Clomiphene Citrate. These drugs trick the brain into stimulating the ovaries to release an egg.
- Step 3: IUI (Intrauterine Insemination): If medicine alone doesn't work, sperm is placed directly inside the uterus during ovulation.
- Step 4: IVF (In Vitro Fertilization): For severe cases, IVF is highly effective. Since women with PCOS have many eggs (high ovarian reserve), they often respond very well to IVF stimulation.
9.3 Pregnancy Complications to Watch
Once pregnant, women with PCOS need extra care. You are at a higher risk for:
- Gestational Diabetes: Since you already have insulin resistance, pregnancy puts extra load on your pancreas.
- Pre-Eclampsia: High blood pressure during pregnancy.
- Early Miscarriage: Due to hormonal imbalances.
Advice: Start taking Pre-natal vitamins and Metformin (if prescribed) before you conceive, not just after.
9.4 Puberty and Menopause
- Teens (Puberty): If your teenage daughter has irregular periods 2 years after her first cycle, do not ignore it as "growing pains." Early diagnosis prevents severe symptoms later.
- Menopause: PCOD doesn't disappear at menopause. While periods stop, the metabolic risks (Diabetes/Heart disease) actually increase as estrogen levels drop.
10. Long-term Complications and Prevention
Many women stop treating their condition once they get married or have a baby. This is a dangerous mistake. PCOS itself is a metabolic syndrome that stays with you for life.
10.1 The Diabetes Connection
India is the Diabetes Capital of the World. A woman with PCOS is 4 times more likely to develop Type 2 Diabetes before the age of 40 compared to a woman without it. The dark patches on your neck (Acanthosis Nigricans) are the warning sign.
10.2 Heart Health and Hypertension
High insulin leads to high cholesterol (specifically High Triglycerides and Low HDL). This clogs arteries over time. By age 50, women with history of untreated PCOS have a significantly higher risk of heart attack or stroke.
10.3 Endometrial Cancer Risk
If you don't have a period for 3-4 months, the lining of your uterus (endometrium) builds up like a thick wall. If this lining is not shed regularly, the cells can become abnormal.
Medical Rule: You must have at least 4-6 periods a year (induced by pills if necessary) to keep the uterine lining thin and healthy.
11. Myths vs. Facts: Busting Common Misconceptions
In India, advice often comes from relatives and neighbors before doctors. Unfortunately, much of this "wisdom" is outdated. Let’s scientifically debunk the biggest myths surrounding PCOD and PCOS.
| MYTH (Galatfehmi) ❌ | FACT (Sachchai) ✅ |
|---|---|
| "Marriage cures PCOD/PCOS." | False. Marriage has no biological effect on ovaries. Regular sexual activity does not regulate hormones. This myth exists because doctors often prescribe birth control pills to brides, which temporarily "fixes" periods. |
| "You cannot get pregnant if you have PCOS." | False. You are not infertile; you just have irregular ovulation. With diet, weight loss, and simple ovulation medicines, most women with PCOS conceive successfully. |
| "Only overweight (fat) women get PCOS." | False. There is a type called "Lean PCOS". Thin women can also have insulin resistance and high testosterone. In fact, Lean PCOS is often harder to diagnose because the patient "looks healthy." |
| "PCOS is just a gynaecological problem." | False. It is an Endocrine (Hormonal) problem. It affects your heart, insulin, brain, and skin, not just your uterus. Treating only the periods is like treating the smoke and ignoring the fire. |
| "You must cut out all carbohydrates (Roti/Rice) forever." | False. You need complex carbs for energy. The goal is to switch from Simple Carbs (Maida/Sugar) to Complex Carbs (Jowar/Bajra/Brown Rice) and control portion sizes. |
12. Conclusion: Taking Charge of Your Health in 2026
We started this guide by asking about the full form of PCOD and PCOS full form. By now, you know that these are not just medical abbreviations—they are messages from your body asking for help.
In the hustle of modern Indian life—managing Zoom calls, household chores, and family expectations—it is easy to ignore that missed period or that sudden weight gain. But remember, your hormones govern your mood, your energy, and your future longevity.
The Good News? You are in control.
PCOS is one of the few medical conditions where the patient has more power than the doctor. 70% of the treatment happens in your kitchen and your gym, not in the clinic.
Don't let the diagnosis define you. Eat real food, move your body, manage your stress, and your body will thank you.
Ready to take the first step?
Do not self-medicate. If you relate to these symptoms, book an appointment with a specialist today. Your health is your greatest wealth.
⚠️ Medical Disclaimer
1. General Information Only: The content provided in this article regarding the full form of PCOD, PCOS full form, symptoms, and treatment is for educational and informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
2. Consult a Specialist: Always seek the advice of your physician, gynaecologist, or other qualified health provider (Registered Medical Practitioner) with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
3. Individual Results May Vary: PCOD and PCOS affect every woman differently. The diet plans, yoga asanas, and home remedies (like seed cycling) mentioned here are general recommendations. What works for one person may not work for another. Please consult a dietician or doctor before making drastic changes to your diet or exercise routine.
4. No Doctor-Patient Relationship: Using this website does not establish a doctor-patient relationship. Reliance on any information provided by this website is solely at your own risk.
5. Emergency: If you think you may have a medical emergency (severe pain, heavy bleeding, etc.), call your doctor or local emergency services immediately.